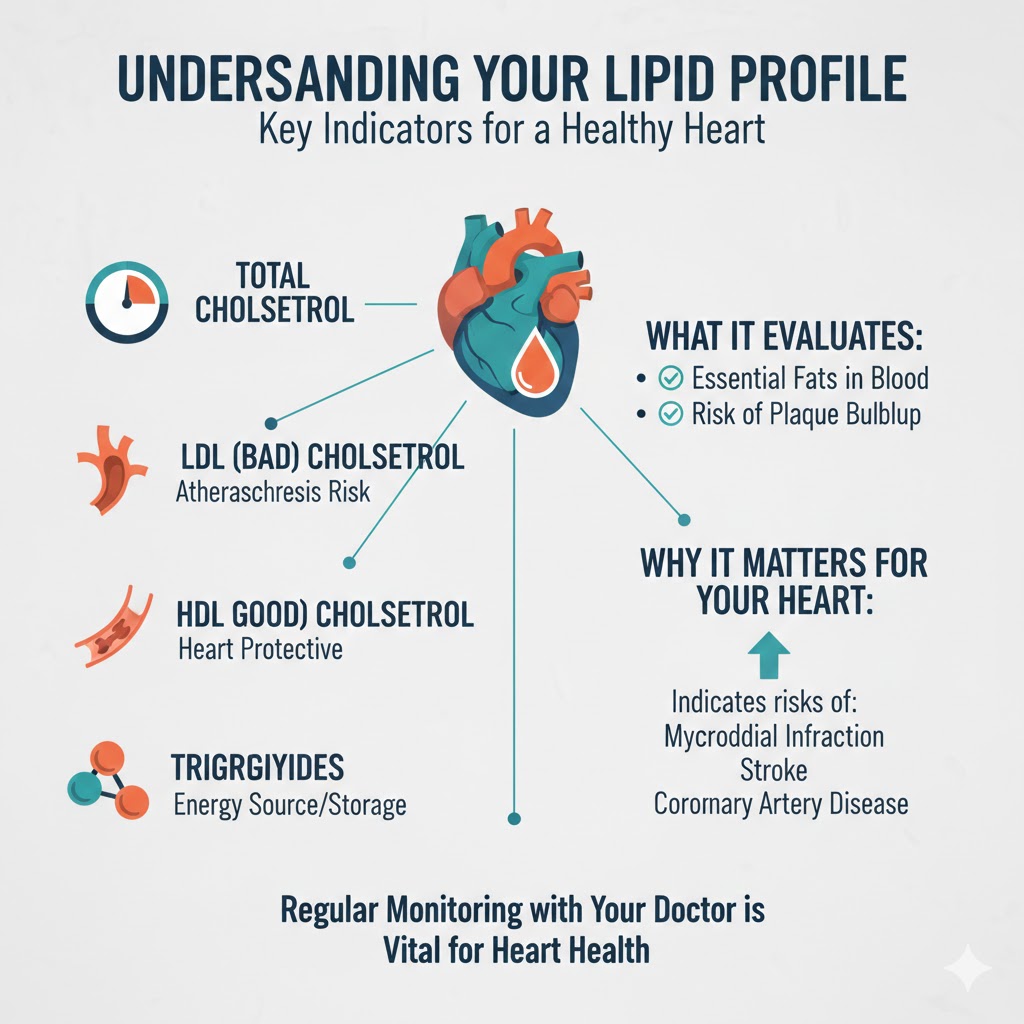
Understanding a lipid profile is vital for monitoring heart health; this blood test evaluates essential fats and may indicate risks of serious health issues.
- Introduction: Understanding the Basics of a Lipid Profile
- What Is a Lipid Profile Test? A Simple Yet Powerful Blood Test
- Lipids explained in everyday language
- Why doctors rely on this test
- Components of a Lipid Profile Explained in Detail
- Total cholesterol
- LDL cholesterol
- HDL cholesterol
- Triglycerides
- Total Cholesterol: What the Overall Number Really Means
- LDL Cholesterol: Why It Is Called “Bad” Cholesterol
- HDL Cholesterol: The Protective “Good” Cholesterol
- Triglycerides: The Often-Ignored Lipid That Matters a Lot
- Why Lipids Are Essential for the Human Body
- What Happens When Lipid Levels Become Imbalanced?
- Dyslipidemia explained
- Why a Lipid Profile Test Is Required Regularly
- Lipid Profile and Heart Health: The Strong Connection
- Who Should Get a Lipid Profile Test and When?
- How Lifestyle Affects Your Lipid Profile Results
- How to Prepare for a Lipid Profile Blood Test
- Understanding Your Lipid Profile Report
- Ways to Maintain a Healthy Lipid Profile Naturally
- Role of Lipid Profile in Preventive Healthcare
- Common Myths and Misconceptions About Lipid Profile Tests
- Conclusion: Making Lipid Profile Testing a Health Habit
- Frequently Asked Questions (FAQs)
Introduction: Understanding the Basics of a Lipid Profile
When it comes to understanding your health, blood tests often act like silent messengers, revealing what’s going on beneath the surface. One such test that plays a major role in preventive healthcare is the lipid profile test. You might have heard your doctor casually say, “Let’s check your lipid profile,” but what does that really mean, and why is it so important to do it regularly?
A lipid profile is not just another routine test—it’s a powerful snapshot of how fats behave inside your body. These fats, known as lipids, are essential for survival. They provide energy, help build cells, and support hormone production. But here’s the catch: when lipid levels go out of balance, they quietly increase the risk of serious health problems, especially heart disease and stroke.
In today’s fast-paced lifestyle, where processed foods, stress, and lack of physical activity have become the norm, lipid disorders are no longer limited to older adults. Even young people are now showing abnormal lipid levels without any obvious symptoms. That’s what makes regular lipid profile testing so crucial—it helps detect hidden risks early, long before they turn into life-threatening conditions.
Think of your lipid profile as a health report card for your heart and blood vessels. It doesn’t just tell you where you stand today, but also gives you a chance to change your future health outcomes. In this article, we’ll break down what a lipid profile is, what each component means, and why checking it regularly can literally save lives.
What Is a Lipid Profile Test? A Simple Yet Powerful Blood Test
A lipid profile test is a blood test that measures different types of fats present in your bloodstream. While the word “lipid” might sound technical, it simply refers to fats and fat-like substances that circulate in your blood. This test is widely used by healthcare professionals to assess your risk of cardiovascular diseases and to monitor overall metabolic health.
What makes the lipid profile test so powerful is its simplicity. With just a small blood sample, usually taken after fasting for 8 to 12 hours, doctors can gather valuable information about how your body processes fats. These fats travel through your blood attached to proteins, forming particles called lipoproteins. The balance between these lipoproteins determines whether fats support your health or slowly harm it.
The lipid profile test typically includes measurements of total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and triglycerides. Each of these plays a unique role in the body. Some help protect your heart, while others, when present in excess, contribute to plaque buildup in arteries.
Doctors often recommend this test as part of routine health checkups, especially for people with risk factors like obesity, diabetes, high blood pressure, smoking habits, or a family history of heart disease. However, even individuals who feel perfectly healthy can benefit from periodic testing because lipid imbalances often develop silently.
In simple terms, a lipid profile test acts like an early warning system. It alerts you to potential problems before symptoms appear, giving you time to make lifestyle changes or seek treatment if necessary.
Components of a Lipid Profile Explained in Detail
A lipid profile is made up of several components, each telling a different part of the story about your health. Understanding these components helps you make sense of your test results rather than feeling overwhelmed by numbers on a report.
Total Cholesterol
Total cholesterol represents the overall amount of cholesterol in your blood. It includes both good and bad cholesterol types. While this number gives a general idea, it doesn’t tell the full story on its own.
LDL Cholesterol
Low-density lipoprotein (LDL) cholesterol is often labeled as “bad” cholesterol. High levels of LDL can lead to cholesterol buildup in artery walls, increasing the risk of heart attacks and strokes.
HDL Cholesterol
High-density lipoprotein (HDL) cholesterol is known as “good” cholesterol. It helps remove excess cholesterol from the bloodstream and transports it to the liver for elimination.
Triglycerides
Triglycerides are another type of fat in the blood, primarily derived from excess calories. High triglyceride levels are linked to an increased risk of cardiovascular disease and metabolic disorders.
Together, these components provide a comprehensive view of how fats are managed in your body. Instead of focusing on a single number, doctors evaluate the balance between these components to assess your overall risk profile.
Total Cholesterol: What the Overall Number Really Means
Total cholesterol is often the first number people notice on their lipid profile report. While it’s tempting to judge your health based solely on this figure, total cholesterol is more like a summary than a detailed explanation. It combines LDL, HDL, and a portion of triglycerides into one value, offering a broad overview of cholesterol levels in your blood.
A normal total cholesterol level is generally considered desirable, but context matters. For example, a person with slightly elevated total cholesterol but high HDL levels may be at lower risk than someone with normal total cholesterol but high LDL levels. This is why doctors rarely rely on total cholesterol alone to make clinical decisions.
Cholesterol itself is not the enemy. Your body needs it to build cell membranes, produce vitamin D, and create essential hormones. Problems arise only when cholesterol, particularly LDL, accumulates excessively in the bloodstream. When this happens, it can stick to artery walls, forming plaques that narrow blood vessels and restrict blood flow.
Monitoring total cholesterol over time helps identify trends. A gradual increase might signal lifestyle issues such as poor diet or reduced physical activity. Regular checks allow early intervention, preventing long-term complications. In essence, total cholesterol acts as a starting point—a signal to look deeper into the individual components of your lipid profile.
LDL Cholesterol: Why It Is Called “Bad” Cholesterol
LDL cholesterol has earned its reputation as “bad” cholesterol for a reason. It carries cholesterol particles from the liver to various tissues in the body. While this process is necessary, excess LDL cholesterol can become dangerous when it starts depositing cholesterol along artery walls.
Over time, these deposits form plaques, a condition known as atherosclerosis. As plaques grow, they narrow the arteries, making it harder for blood to flow freely. This increases blood pressure and raises the risk of heart attacks and strokes. In severe cases, plaques can rupture, leading to sudden and life-threatening events.
What makes LDL cholesterol particularly concerning is that high levels usually don’t cause noticeable symptoms. You could feel perfectly fine while silent damage is occurring inside your blood vessels. This is why regular lipid profile testing is so important—it helps identify elevated LDL levels before complications arise.
Diet plays a major role in LDL levels. Foods high in saturated fats, trans fats, and refined carbohydrates can raise LDL cholesterol. On the other hand, physical activity, fiber-rich foods, and healthy fats can help lower it. For some individuals, genetics also influence LDL levels, making regular monitoring even more essential.
HDL Cholesterol: The Protective “Good” Cholesterol
HDL cholesterol is often referred to as the “good” cholesterol, and unlike LDL, higher levels of HDL are generally beneficial. HDL acts like a cleanup crew in your bloodstream. It collects excess cholesterol from artery walls and transports it back to the liver, where it can be processed and eliminated from the body.
This protective role makes HDL a critical factor in reducing cardiovascular risk. Even if someone has moderately high LDL cholesterol, having high HDL levels can help counterbalance some of that risk. That’s why doctors often look at the ratio between total cholesterol and HDL rather than focusing on isolated numbers.
Lifestyle habits have a strong influence on HDL levels. Regular physical activity, especially aerobic exercise, can significantly increase HDL cholesterol. Healthy fats from sources like nuts, seeds, and olive oil also support higher HDL levels. Avoiding smoking is another key factor, as smoking tends to lower HDL cholesterol.
It’s important to understand that not all cholesterol is harmful. HDL cholesterol proves that balance matters more than elimination. Rather than trying to reduce cholesterol to zero, the goal is to maintain a healthy balance that supports long-term heart health.
Triglycerides: The Often-Ignored Lipid That Matters a Lot
Triglycerides are a type of fat that often receive less attention than cholesterol, but they play a crucial role in your lipid profile. These fats come from excess calories that your body doesn’t immediately need for energy. Instead of wasting them, your body stores these calories as triglycerides in fat cells.
While triglycerides are essential for energy storage, high levels can be harmful. Elevated triglycerides are linked to an increased risk of heart disease, pancreatitis, and metabolic conditions such as type 2 diabetes. High triglyceride levels often go hand in hand with other health issues like obesity, insulin resistance, and low HDL cholesterol.
One of the main reasons triglycerides rise is an unhealthy lifestyle. Diets high in sugar, refined carbohydrates, and alcohol can significantly increase triglyceride levels. Lack of physical activity further worsens the problem. Unlike cholesterol, triglyceride levels can fluctuate quickly based on recent eating habits, which is why fasting is often required before the test.
Regular lipid profile testing helps track triglyceride levels and identify patterns. If levels remain consistently high, it’s a clear sign that lifestyle changes are needed. Addressing triglycerides early can greatly reduce the risk of future cardiovascular complications.
Why Lipids Are Essential for the Human Body
Lipids often get a bad reputation because they are associated with weight gain and heart disease, but the truth is far more balanced. Lipids are absolutely essential for normal body function. Without them, life as we know it would not be possible. The key is not eliminating lipids, but maintaining them at healthy levels.
At the most basic level, lipids are a major source of energy. When your body needs fuel, especially during rest or prolonged activity, it turns to stored fats for long-lasting energy. Unlike carbohydrates, which burn quickly, lipids provide a slow and steady energy supply that keeps the body functioning efficiently.
Lipids also play a structural role. Every cell membrane in your body is made largely of lipids. These membranes protect cells and control what enters and exits them. Without adequate lipids, cell integrity would be compromised, affecting organs, tissues, and overall health.
Hormone production is another critical function of lipids. Many essential hormones, including steroid hormones, are derived from cholesterol. These hormones regulate growth, metabolism, stress response, and reproductive health. Low or imbalanced lipid levels can disrupt hormonal balance, leading to a range of health issues.
Additionally, lipids help absorb fat-soluble vitamins such as vitamins A, D, E, and K. These vitamins are crucial for vision, bone health, immune function, and blood clotting. Without proper lipid levels, your body cannot absorb these nutrients effectively, even if your diet is otherwise healthy.
Understanding the essential role of lipids helps shift the focus from fear to balance. A lipid profile test doesn’t aim to eliminate fats but ensures they are working for you—not against you.
What Happens When Lipid Levels Become Imbalanced?
When lipid levels drift outside their healthy range, the condition is known as dyslipidemia. This imbalance can involve high LDL cholesterol, low HDL cholesterol, elevated triglycerides, or a combination of these. Dyslipidemia is one of the most significant risk factors for cardiovascular disease worldwide.
The most dangerous aspect of lipid imbalance is that it develops silently. You won’t feel pain or discomfort as cholesterol slowly accumulates in your arteries. Over time, these fatty deposits harden and narrow blood vessels, reducing blood flow to vital organs like the heart and brain. This process can take years or even decades before symptoms appear.
Imbalanced lipid levels are strongly linked to heart attacks and strokes. When blood flow to the heart is blocked, it can cause chest pain or a heart attack. When blood flow to the brain is interrupted, it can result in a stroke. Both conditions can be life-threatening or lead to long-term disability.
Beyond heart health, abnormal lipid levels also affect metabolic health. High triglycerides are often associated with insulin resistance and type 2 diabetes. Fatty liver disease, another growing health concern, is also closely linked to elevated lipid levels.
The good news is that lipid imbalances are often reversible, especially when detected early. Regular lipid profile testing makes it possible to identify problems before irreversible damage occurs, giving you the opportunity to take control of your health.
Why a Lipid Profile Test Is Required Regularly
Regular lipid profile testing is essential because lipid levels change over time. Age, diet, physical activity, stress, weight changes, and medical conditions all influence how your body processes fats. A test done once in your lifetime cannot accurately represent your long-term health status.
One of the biggest reasons for regular testing is early detection. Many people first discover abnormal lipid levels only after experiencing a heart-related event. Routine testing helps catch problems early, when lifestyle changes alone may be enough to correct them.
Another important reason is risk assessment. Doctors use lipid profile results to calculate cardiovascular risk and decide whether preventive measures are needed. This could include dietary changes, exercise recommendations, or medical treatment when necessary.
For individuals already diagnosed with high cholesterol, diabetes, or hypertension, regular lipid testing helps monitor progress. It shows whether current treatment or lifestyle adjustments are working or if changes are needed.
Even people who feel healthy benefit from periodic testing. Modern lifestyles have increased the prevalence of hidden risk factors. Regular lipid profile checks act like a maintenance check for your body—small effort, big payoff.
Lipid Profile and Heart Health: The Strong Connection
The relationship between lipid profile results and heart health is well established. Cardiovascular diseases remain one of the leading causes of death globally, and abnormal lipid levels are one of the primary contributors.
High LDL cholesterol and triglycerides promote plaque formation in arteries, while low HDL cholesterol reduces the body’s ability to remove excess cholesterol. This combination accelerates the development of atherosclerosis, making heart disease more likely.
Doctors often rely on lipid profile results to determine heart disease risk even before symptoms appear. This allows for preventive strategies rather than reactive treatment. Lowering LDL cholesterol and triglycerides while increasing HDL cholesterol has been shown to significantly reduce the risk of heart attacks and strokes.
In many ways, the lipid profile serves as a roadmap for heart health. It highlights problem areas and guides decisions that protect the heart over the long term.
Who Should Get a Lipid Profile Test and When?
While lipid profile testing is beneficial for everyone, certain groups need it more urgently. Adults are generally advised to have their lipid profile checked every four to six years, starting in early adulthood. However, individuals with risk factors may need more frequent testing.
People with a family history of heart disease, high cholesterol, or stroke should begin testing earlier. Those with conditions such as diabetes, obesity, high blood pressure, or thyroid disorders are also at higher risk of lipid abnormalities.
Lifestyle factors matter too. Smokers, individuals with sedentary habits, and those consuming diets high in processed foods should consider regular testing regardless of age.
Ultimately, lipid profile testing is not just for those who are sick—it’s for anyone who wants to stay healthy.
How Lifestyle Affects Your Lipid Profile Results
Your lifestyle has a powerful impact on lipid levels. What you eat, how active you are, how well you sleep, and how you manage stress all influence your lipid profile.
Diets high in saturated fats, trans fats, and sugar tend to raise LDL cholesterol and triglycerides. In contrast, diets rich in fruits, vegetables, whole grains, lean proteins, and healthy fats help maintain balanced lipid levels.
Physical activity increases HDL cholesterol and helps lower LDL and triglycerides. Even moderate exercise, such as brisk walking, can make a measurable difference.
Stress and poor sleep also play a role. Chronic stress can negatively affect lipid metabolism, while inadequate sleep is linked to higher triglyceride levels.
The lipid profile is, in many ways, a reflection of daily habits. Regular testing helps you see the real impact of your lifestyle choices.
How to Prepare for a Lipid Profile Blood Test
Preparing properly for a lipid profile test ensures accurate results. Most doctors recommend fasting for 8 to 12 hours before the test, meaning no food or sugary drinks during that time. Water is usually allowed.
Avoid heavy meals, alcohol, and intense exercise the day before the test, as these can temporarily affect lipid levels. Inform your healthcare provider about any medications you are taking, as some drugs can influence results.
Simple preparation leads to reliable results, which in turn lead to better health decisions.
Understanding Your Lipid Profile Report
A lipid profile report may look confusing at first, but it becomes easier to understand when broken down. Each component is listed with a value and a reference range indicating whether it falls within normal limits.
Doctors don’t just look at individual numbers—they evaluate patterns and ratios. For example, the balance between LDL and HDL is often more important than total cholesterol alone.
Discussing your results with a healthcare professional helps put them into context. They can explain what the numbers mean for your specific health situation and recommend next steps if needed.
Ways to Maintain a Healthy Lipid Profile Naturally
Maintaining a healthy lipid profile doesn’t always require medication. In many cases, natural lifestyle changes are highly effective.
- Eat a balanced diet rich in fiber and healthy fats
- Exercise regularly
- Maintain a healthy weight
- Avoid smoking
- Limit alcohol consumption
- Manage stress effectively
Consistency is key. Small, sustainable changes often lead to long-term improvements in lipid levels.
Role of Lipid Profile in Preventive Healthcare
Preventive healthcare focuses on stopping disease before it starts, and the lipid profile is a cornerstone of this approach. By identifying risks early, it allows individuals to take control of their health proactively.
Regular lipid testing empowers informed decision-making and reduces the burden of chronic diseases on individuals and healthcare systems alike.
Common Myths and Misconceptions About Lipid Profile Tests
Many people believe lipid tests are only necessary for older adults or those with symptoms. In reality, lipid abnormalities can affect anyone at any age.
Another myth is that cholesterol is always bad. As discussed earlier, cholesterol plays essential roles in the body—the problem lies in imbalance, not presence.
Clearing these misconceptions encourages more people to take preventive testing seriously.
Conclusion: Making Lipid Profile Testing a Health Habit
A lipid profile test is much more than a routine blood test—it’s a window into your heart health and overall well-being. By understanding what a lipid profile is and why it needs to be checked regularly, you empower yourself to make smarter health choices.
Regular testing helps detect hidden risks, guides lifestyle changes, and prevents serious health complications before they arise. In a world where chronic diseases are increasingly common, making lipid profile testing a habit is a simple yet powerful step toward a healthier future.
Frequently Asked Questions (FAQs)
1. How often should a lipid profile be checked?
Most adults should check it every 4–6 years, or more often if risk factors are present.
2. Is fasting always required for a lipid profile test?
Fasting is commonly recommended, especially for accurate triglyceride levels.
3. Can young people have abnormal lipid profiles?
Yes, lifestyle and genetics can affect lipid levels at any age.
4. Can lipid levels improve without medication?
In many cases, lifestyle changes alone can significantly improve lipid levels.
5. What is the most important lipid profile component?
All components matter, but the balance between LDL and HDL is especially important.